If you’ve been told you have Burning Mouth Syndrome (BMS) or you’re supporting someone who has it, you will know how frustrating it can be to experience a persistent burning, tingling or scalding sensation in the mouth without visible signs of injury. As a physician specializing in oral medicine with over a decade of experience, my goal is to explain recent developments in the treatment of BMS in plain Language, so you and your caregivers feel informed and empowered.
You might already have come across articles such as “Burning Mouth Syndrome Natural Treatment,” “Burning Mouth Syndrome Dietary Supplement,” or “Burning Mouth Syndrome All Natural Organic Supplements.” These topics are often discussed, but it’s important to separate what’s promising from what’s proven. What is the new treatment for Burning Mouth Syndrome? Let’s walk through what BMS is, why finding a new treatment matters, what the most up-to-date options are (including a genuinely new one), and what you can expect moving forward.
What is Burning Mouth Syndrome?
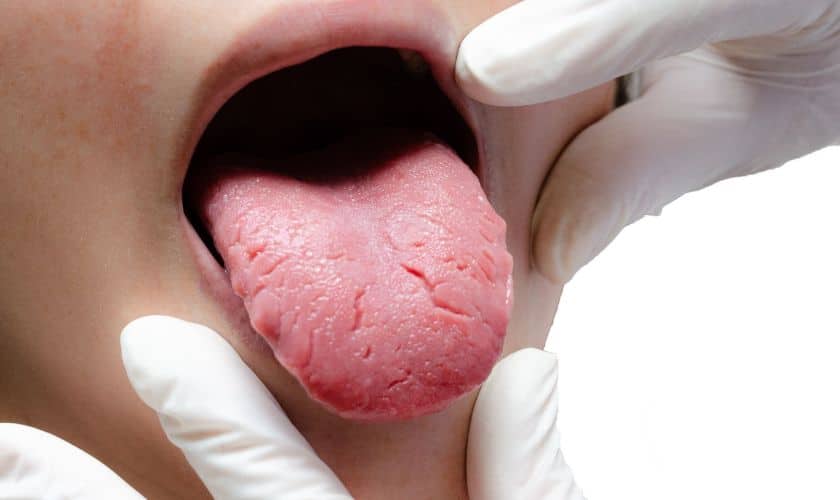
BMS is a chronic condition where you feel a burning, scalding, or tingling sensation in your tongue, lips, gums, pal, or other parts of the mouth (and sometimes throat). Still, when your doctor or dentist looks inside your mouth, they often cannot see a tissue problem that fully explains your discomfort.
Key features:
- The pain or burning often has no obvious cause (we call this primary BMS), or it may follow another condition such as dry mouth, nutritional deficiency, or poorly fitting dentures (we call this secondary BMS).
- The burning may start somewhat unbeknownst to you, and it often becomes more noticeable as the day progresses.
- It is more common in women, especially during or after the menopausal years.
- Because the cause (or causes) are often not clear, treatment can feel slow and frustrating; there is no universal cure yet.
Why does it matter? The constant sensation of burning or stinging can affect how you eat, speak, drink, and even sleep. It may also lead to anxiety or low mood, especially when the cause isn’t clear or relief is slow. Patient-centered care demands that we look not only at treating the symptoms, but also at supporting your quality of life.
Traditional Treatment Options
Before we look at new developments, let’s summarize what has been used so far, so you understand the landscape.
Diagnosis and addressing underlying causes
- Your dentist or doctor will first check for local or systemic causes: e.g., infections, vitamin deficiencies (B12, folate, iron, zinc), dry mouth, thyroid problems, diabetes, and oral irritants.
- If there is a clear cause (secondary BMS), addressing that cause can relieve the symptoms. For example: treating a fungal infection, correcting a nutritional deficit, or removing an irritant.
Symptom-based treatments
When no clear cause emerges (primary BMS) or even alongside cause-based treatments, symptom relief is the focus. Some of the common options include:
- Saliva substitutes or sprays if dry mouth is present.
- Topical oral rinses with lidocaine (a local anesthetic) to reduce burning.
- Systemic medications used in nerve-pain settings: e.g., benzodiazepines (such as clonazepam), tricyclic antidepressants (amitriptyline), anticonvulsants (gabapentin).
- Nutritional supplements if deficiencies are present (or suspected) – e.g., B-vitamins, zinc.
- Non-drug approaches: cognitive behavioral therapy for symptoms of anxiety or coping with chronic pain.
Limitations of traditional treatments
- The evidence for many treatments is modest in quality: small trials, variable methods, inconsistent outcomes.
- Many patients find that relief is partial rather than full.
- Some treatments have side effects (for example, sedative effect of benzodiazepines) or may not be suitable for all patients.
What is the New Treatment?
The exciting piece of news is that researchers have recently studied a combination of therapies that may offer better relief than the older approaches alone.
Photo bio modulation (PBM) combined with Oral Cry therapy (OCT)
- Photo bio modulation (also called low-level laser therapy or LLLT) is a technique where low-intensity light is applied to approximate the area of pain or burning in the mouth. A 2024 news article reported a ten-week study in which PBM significantly lowered pain scores in BMS patients.
- More recently (2025), a multi-institutional randomized controlled trial compared: PBM alone, OCT alone, PBM + OCT, and drug therapy (DT) alone in patients with BMS. The PBM + OCT combination achieved an 81.25% response rate after seven weeks — nearly five times greater pain-reduction than the drug therapy alone. Additionally, anxiety symptoms improved significantly.
- Oral Cry therapy (OCT) involves cooling the oral mucosa with a safe, non-invasive method (often cold fluid or chill surface contact). The combined approach appears to address both the sensory neuropathy of BMS and the associated anxiety component.
- There were no serious adverse events reported in that trial. The authors concluded this combination is a “promising pain-management option” for BMS.
So,o in answer to your question “what is the new treatment for burning mouth syndrome?” — it is the combination therapy of PBM plus OCT. It is not yet widely availableeverywheree;e, it will likely require referral to a specialist clinic or dentist with access to laser therapy equipment, and it may be more costly. But the early results are encouraging and represent a meaningful advance beyond older treatments.
How Does This New Treatment Work, and What You Should Know
Mechanism
- BMS is thought to involve neuropathic changes (nerve damage or dysfunction) in the mouth’s sensory system — for instance, damaged taste fibers, altered pain signaling,an d reduced inhibition of nerve firing.
- PBM is believed to stimulate cellular repair, reduce inflammation, regulate nerve-cell activity, and modulate oxidative stress. For example, one study on diode laser therapy in BMS showed reductions in saliva biomarkers of inflammation.
- OCT adds a cooling effect to reduce nerve excitation, swellin,swellingain signaling. When combined with PBM, the effect appears greater than either alone.
Practical Considerations
- Because this is a new protocol, not every clinic offers it. You may need referral to a specialist in oral medicine, pain management, or an advanced dentist.
- It may require multiple sessions (e.g., the trial useda 7-week period with follow-up) and possibly ongoing maintenance.
- Stay aware of cost, travel time, and whether your dental insurance (if applicable) covers it.
- Before undergoing, you should ask: what are the expected number of sessions, how long for each, what clinical outcomes are likely, what side-effects or limitations.
- It is not a guaranteed cure, but for many people it may provide better relief than older approaches.
- It complements rather than replaces other care — you’ll still need good oral hygiene, check for underlying causes, and possibly maintain lifestyle and nutritional supports.
Who Might Benefit Most
- Patients who have already tried older treatments (topical, systemic meds, supplements) without adequate relief.
- Patients with bothersome anxiety or mood changes related to BMS, since the recent study found improved anxiety scores with the PBM + OCT combo.
- Patients in sufficiently good overall health to tolerate repeated sessions and who are willing to commit to the process.
Limitations and Things to Be Clear On
- Because it is relatively new, long-term outcomes are still under study. The 2025 trial followed up for 12 weeks; more extended data are needed.
- It may not be suitable or effective for all types of BMS, especially if the pain is due primarily to an underlying cause (secondary BMS) rather than neuropathic change.
- Access may be limited in some regions — you might need to consult a well-informed specialist.
- Even with treatment, you may still need to manage triggers (diet, dry mouth, stress) and use supportive therapies.
Supporting Therapies You Can Use
While you explore the new treatment option, you can work on supporting therapies and lifestyle adjustments to complement whatever treatment you and your clinician decide on. These also help you prepare for and optimize the results of any intervention.
Diet and Oral Habits
- Avoid irritating foods and drinks: acidic beverages (orange juice, carbonated drinks), spicy foods, very hot foods, alcohol, products containing mint or cinnamon. These may trigger or worsen burning sensations.
- Keep your mouth well hydrated: sip water, use sugar-free gum or ice chips if dry mouth is present.
- Ensure your dentures (if you wear any) fit correctly and are well-maintained to avoid mechanical irritation.
Nutritional Support and Supplements
- While not a replacement for medical treatment, certain nutritional supports may help: check your levels of vitamin B12, folate, iron, zinc ,and correct if deficient.
- One of the better-studied supplements is Alpha-Linolenic Acid (ALA). Research suggests that ALA may reduce pain in some BMS patients. For example, a systematic review found favorable outcomes (though the quality of evidence varies).
- If you are investigating “Burning Mouth Syndrome Dietary Supplement” or “Burning Mouth Syndrome All Natural Organic Supplements”, do so with caution and under professional guidance: supplements are not regulated the same way as medications, and what works for one person may not work for another.
- Always inform your healthcare provider of any supplement you take — there may be interactions with other medications or underlying conditions.
Stress, Sleep, and Mental Well-being
- Because chronic pain often worsens with stress, anxiety, or poor sleep, build in self-care practices: gentle exercise, relaxation, mindfulness, and good sleep hygiene.
- If you experience anxiety or mood changes, consider speaking with a counseling professional or your dentist/doctor about support.
- Keeping a symptom diary (what you ate, what you drank, what made the burning better or worse) can help you and your clinician recognize patterns.
Oral Hygiene and Regular Dental Care
- Use mild, non-irritant toothpaste (avoid strong mint flavors, cinnamon).
- Maintain regular dental check-ups to ensure no new oral issues contribute to the burning sensation (infections, changes in denture fit, etc.).
- Make sure you use alcohol-free mouthwashes if you have dry mouth or irritation.
How to Discuss This With Your Healthcare Team
Here’s how to talk with your dentist or doctor about making use of the new treatment plus supporting measures:
- Explain your symptoms clearly: When did they start, how long do they last, do they get worse at certain times or after certain foods, is there dryness or a taste change?
- Ask about testing: Have you been tested for deficiencies (B12, iron, zinc), dry mouth, thyroid, diabetes, or other possible underlying causes of secondary BMS?
- Mention the new treatment: Say something like: “I’ve read about the combination of Photo bio modulation and Oral Cryotherapy as a newer treatment for BMS — could that be an option for me?”
- Understand the logistics: If your provider thinks it is appropriate, ask how many sessions you might need, how long each session lasts, what the cost is, and how they measure success (change in pain scale, quality of life).
- Plan the overall approach: Ask how supporting therapies (diet, hydration, supplements, stress reduction) will be incorporated alongside the main treatment.
- Set expectations: Recognize that relief may be gradual, you may need multiple sessions and supportive therapies, and no treatment is guaranteed to fully cure BMS at this stage.
- Follow-up and adjust: After starting treatment, plan follow-up visits to assess progress, complications, or side effects, and revisit other strategies if needed.
Summary
If you or a loved one has BMS, you’re not alone — it’s a challenging condition, but the good news is that progress is happening. The most promising new treatment is the combination of Photo bio modulation (PBM) plus OraCryotherapy (OCT). This represents a step beyond earlier therapies and may offer better relief for many people. But it’s not a standalone miracle: you’ll get the best results by pairing it with the fundamentals — investigating underlying causes, managing your diet and hydration, addressing stress and sleep, and working with your healthcare team.
If you’re considering the “Burning Mouth Syndrome Natural Treatment” or “Burning Mouth Syndrome Dietary Supplement” or “Burning Mouth Syndrome” or “All Natural Organic Supplements”, do so within a broader plan and always under professional supervision. For anyone asking “what is the new treatment for burning mouth syndrome?” — now you have a clear answer and a frame for next steps.