Azoospermia is a condition characterized by the absence of sperm in a man’s semen, making natural conception challenging. Diagnosing azoospermia is the first step in understanding the underlying cause and deciding on possible treatment options. This guide will outline the diagnostic procedures, tests involved, and what to expect throughout the process.
Why Diagnose Azoospermia?
A diagnosis of azoospermia can reveal crucial details about a man’s reproductive health, helping to identify whether the cause is obstructive or non-obstructive. Determining the type of azoospermia is essential for recommending the appropriate treatment and evaluating fertility options, including assisted reproductive technologies.
Initial Evaluation and Medical History
The diagnostic process often begins with a comprehensive medical history and physical examination conducted by a reproductive specialist or urologist. Understanding the patient’s health history and lifestyle factors can provide clues about possible causes of azoospermia, including:
- Previous surgeries (such as vasectomy)
- Infections or injuries
- Exposure to toxins
- Genetic conditions or family history
- Lifestyle habits (smoking, substance use, etc.)
Semen Analysis: The First Step
The first and most critical test in diagnosing azoospermia is a semen analysis. This test is typically repeated at least twice to confirm the absence of sperm in the ejaculate.
Procedure:
- The patient provides a semen sample, usually through masturbation, which is analyzed in a lab.
- The sample is examined under a microscope to check for the presence of sperm and to measure volume, pH, and white blood cell count.
If no sperm are detected, further diagnostic tests are recommended to determine if the azoospermia is due to a blockage (obstructive) or a problem with sperm production (non-obstructive).
Hormone Testing
Hormone analysis helps to understand if there’s a hormonal cause for azoospermia, which is more common in cases of non-obstructive azoospermia.
Common hormones tested include:
- FSH (Follicle-Stimulating Hormone): Elevated levels may indicate an issue with sperm production.
- LH (Luteinizing Hormone): High LH levels often suggest a testicular problem.
- Testosterone: Low levels may contribute to low sperm production.
- Prolactin: Elevated prolactin levels can interfere with fertility and testosterone production.
What to Expect: Hormone testing is a simple blood test. If abnormal hormone levels are found, they might indicate non-obstructive azoospermia, guiding the specialist toward possible hormonal treatments.
Genetic Testing
Since certain genetic conditions are linked to azoospermia, genetic testing may be recommended, especially if non-obstructive azoospermia is suspected.
Common genetic tests include:
- Y Chromosome Microdeletion Testing: Checks for deletions on the Y chromosome that may impair sperm production.
- Karyotype Analysis: Detects chromosomal abnormalities, such as Klinefelter syndrome, a common cause of non-obstructive azoospermia.
- Cystic Fibrosis (CF) Gene Mutation Testing: Identifies mutations that may cause congenital absence of the vas deferens, leading to obstructive azoospermia.
What to Expect: Genetic testing typically involves a blood sample. The results may take a few weeks, as they require specialized analysis. Genetic counseling may also be recommended to discuss potential impacts on fertility and offspring.
Imaging Tests
Imaging techniques help visualize any structural abnormalities or blockages in the reproductive tract. Common imaging tests include:
- Scrotal Ultrasound: Assesses the structure of the testes and epididymis, detecting signs of obstruction or abnormalities like varicoceles.
- Transrectal Ultrasound (TRUS): Used to visualize the prostate, seminal vesicles, and ejaculatory ducts, particularly helpful in diagnosing obstructive azoospermia.
- MRI or CT Scan: In rare cases, more detailed imaging may be necessary, especially if other abnormalities are suspected.
What to Expect: Ultrasound tests are non-invasive and painless, usually completed within 15-30 minutes. TRUS involves a small probe inserted into the rectum, which may cause slight discomfort.
Testicular Biopsy
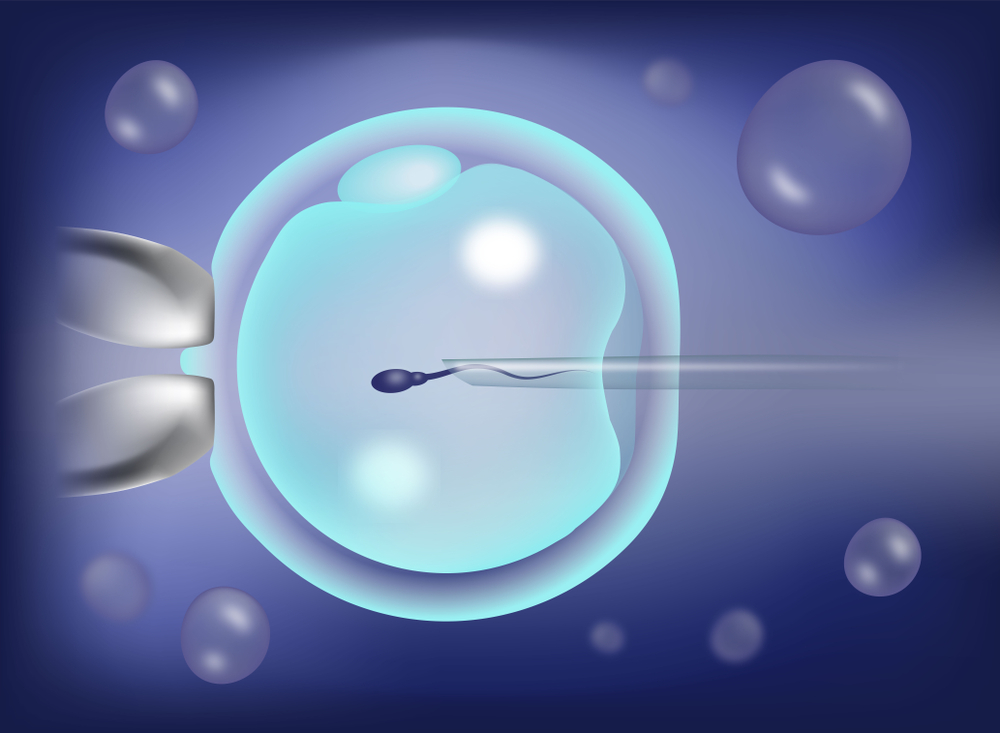
For non-obstructive azoospermia cases, a testicular biopsy may be performed to assess whether any sperm are being produced within the testes, which could be retrieved for assisted reproductive treatments like IVF.
Types of Biopsies:
- Fine Needle Aspiration: A small needle extracts tissue samples, offering a less invasive option.
- Open Testicular Biopsy: In this more thorough procedure, a small incision is made in the scrotum to remove tissue for examination.
What to Expect: Testicular biopsy is often performed under local anesthesia. Recovery is quick, though patients may experience minor discomfort for a few days.
Diagnostic Summary and Next Steps
After completing these tests, the results will indicate whether the azoospermia is obstructive or non-obstructive. Here’s a summary of potential outcomes and subsequent steps:
| Diagnostic Test | Possible Outcome | Next Steps |
|---|---|---|
| Semen Analysis | Confirms azoospermia | Proceed to further testing |
| Hormone Testing | Hormonal imbalance detected | Consider hormone therapy |
| Genetic Testing | Genetic cause identified | Discuss genetic counseling |
| Imaging Tests | Structural abnormality found | Possible surgical correction |
| Testicular Biopsy | Sperm present in testes | Possible sperm retrieval & IVF |
Conclusion
Diagnosing azoospermia involves a series of tests to understand its type and underlying cause. The diagnostic pathway can seem daunting, but each test provides essential information to guide treatment options and fertility possibilities. By working closely with a specialist and following through with the recommended tests, men with azoospermia can explore paths toward effective treatment and even fatherhood through assisted reproductive options.